The top three EHR implementation challenges faced by practices
EHR systems are vital for modern healthcare, but implementing them isn’t always straightforward. Transitioning from paper-based systems or upgrading to a more sophisticated EHR comes with hurdles. Below, we explore three key EHR implementation challenges, alongside practical strategies to overcome them.
Staff resistance to change
People generally have a difficult time accepting change, especially within the work environment. Likely, there will be resistance to this change from the clinical and support staff all the way up to the board members and stakeholders.
The EHR implementation process must be delivered with a promotion and marketing plan to champion the change, and clinicians should be invited into vendor selection and workflow design to improve buy-in.
Plan your implementation successfully with this customizable EHR implementation template
Address staff resistance by communicating the benefits of the EHR system early and often. Develop a comprehensive EHR implementation plan that includes clear communication strategies to highlight how the new system will positively impact workflows.
Training:
Slow and steady implementation combined with ongoing, hands-on training is crucial. Staff should be assured that while the learning curve may cause temporary slowdowns, the new system will ultimately help them work more efficiently. Include role-specific training (physicians, nurses, front desk) and realistic, task-based scenarios that mirror day-to-day work to reduce frustration and reduce EHR data entry burden.
Engagement:
Create a culture of openness where concerns can be aired. Offering channels for feedback and updates on the system's performance encourages staff to invest in the EHR transition.
Resistance often stems from fears of disruption to daily routines. However, by emphasizing how the system enhances the practice's overall efficiency, improves patient care, and may even lead to better job satisfaction, you can reduce this challenge.
Also highlight usability improvements and any planned steps to reduce documentation workload (templates, macros, scribes) to address common issues with EHR systems and EHR data entry.
Lost productivity and incomplete implementation
One of the biggest problems with EHR implementation is the temporary dip in productivity. Practices should prepare for reduced patient flow and workflow efficiency in the short term, which is a natural consequence of adopting new technologies.
Lost productivity is a major concern when staff are learning to use a new system. This is especially concerning when practice's main motivation for implementing a system is reportedly to increase efficiency. Even when an EHR is “live,” old habits can die hard. Staff might continue documenting on paper or using outdated methods, which leads to inefficiencies.
Solution:
Set clear expectations about reduced productivity during the training period. To mitigate losses, consider temporary staffing solutions or overtime pay. Some EHR vendors provide support services during the go-live phase, which can reduce the workload on your in-house team.
Monitor simple operational metrics (visit length, check-in to check-out time, chart close rates) so you can quantify the impact and respond quickly.
Preventing workarounds:
Incomplete implementation occurs when employees revert to older methods. For example, staff might document patient data on paper instead of entering it directly into the system. This creates twice the work and diminishes the benefits of the EHR. Prevent this by ensuring comprehensive training and demonstrating how the EHR can streamline daily tasks.
Demonstrate to employees how the system improves workflow and patient outcomes (or hire an EHR consultant to do it), which aligns with the initial project goals of efficiency and improved care.
Note on infrastructure: Most EHRs are now cloud-first, which means less on-site storage space is needed for EHR systems and fewer local servers to maintain, but ensure your network, bandwidth, and backup strategies are sufficient before go-live.
Data migration difficulties
Migrating existing data to a new EHR can be a tedious and error-prone process. This data must be migrated accurately to avoid disruptions in patient care.
- Prioritize records: Practices must decide how far back to go with data migration. Begin by prioritizing the most recent and critical records to ensure that clinicians have access to the most current patient data.
- Assign a point person: To manage ongoing data entry, designate a team member responsible for processing all new information coming in via fax, email, or paper documentation. This ensures new patient information is promptly entered into the EHR, reducing the chances of errors or delays.
- Validation processes: Data integrity is paramount when dealing with sensitive medical information. Setting up validation processes and regular audits throughout the migration can help catch errors early, ensuring that patient records are complete and accurate. Map codes (ICD, CPT), reconcile medication lists, and establish data governance rules so data will support later EHR data analytics and quality reporting.
Strategies to overcome EHR implementation challenges
While these are the three most common challenges of EHR implementation, there are proactive steps your practice can take to ensure a smoother transition:
- Comprehensive training: Invest time in training to ensure all staff are comfortable with the new system. Regularly scheduled refresher courses can help maintain proficiency and adapt to updates in the software.
- Realistic timelines: Avoid rushing the implementation. Create a timeline that allows for a gradual rollout, enabling staff to learn and adapt without overwhelming them.
- Vendor support: Utilize the resources provided by your EHR vendor. Many offer on-site support during the critical initial phase of implementation. Review contract language and confirm the scope of support, uptime guarantees, and data portability clauses before signing.
- Patient communication: Inform your patients about the transition to an EHR system. This can help manage their expectations during the adjustment period and highlight the benefits they will experience, such as more efficient appointment scheduling and faster access to their records.
- Measure and iterate: Collect baseline metrics and track progress (productivity, chart completion, patient wait times, safety events). Use that data to prioritize quick wins and continuous improvements, including preparing your data so it can be used for reporting and EHR data analytics.
Free white paper

EHR Implementation Template
Get all the planning tools you need to make your EHR implementation a success

Featured white papers
Related articles
-

Paper Charting to EHR Software: 4 Common Mistakes
Prepare for the challenges ahead by learning from these common mistakes practices make during the...
-

Introducing "Actions": The AI-Powered Tool That’s Transforming Primary Care Workflows
70% of clinicians are reporting better focus & engagement with their patients thanks to Elation H...
-
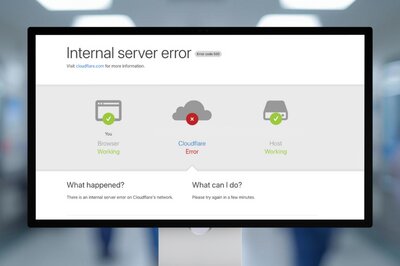
Four coping strategies for unplanned EHR system downtime
What you need to do to keep your practice running smoothly during EHR system downtime


